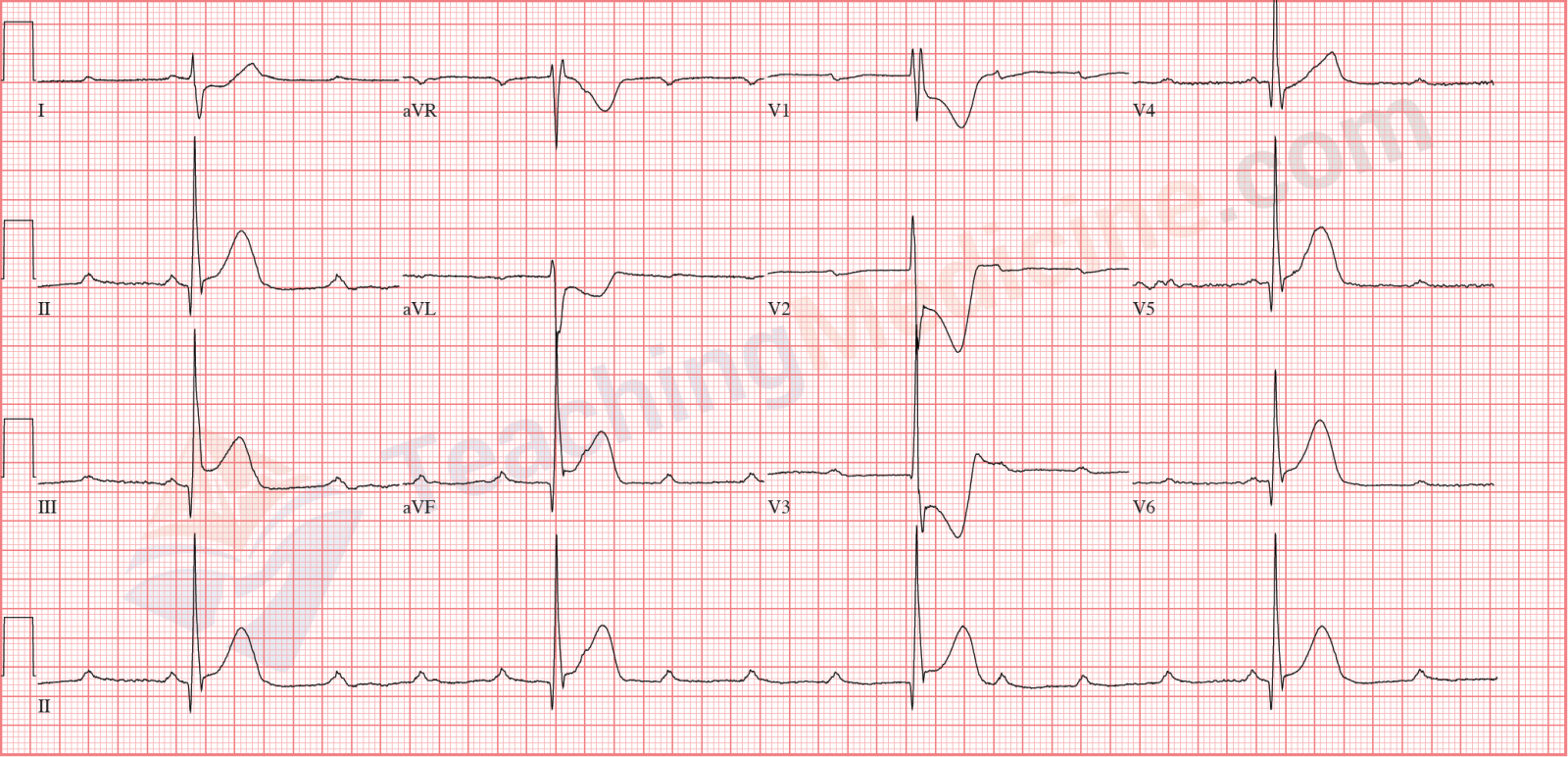
Junctional Rhythm Diagnostic criteria: (boldfaced with * indicates an important feature)- Rate: typically 40-60
- Rhythm: regular
- * P waves: present, usually inverted or absent
- * PR interval: short (if P wave is in front of QRS), or "not applicable" if P wave is AFTER QRS
- QRS: narrow
ElectrophysiologyA junctional pacemaker originates in the AV node. The AV node sits between the atria and the ventricles and so is at the "junction".The rate is slower than the SA node. This is because the phase 4 of the action potential is more shallow compared to the SA node and therefore, the time to reach the action potential threshold takes longer. Therefore, the frequency of firing is less and the heart rate is less.
There are 3 typical appearances of a junctional rhythm.
P wave before QRS: 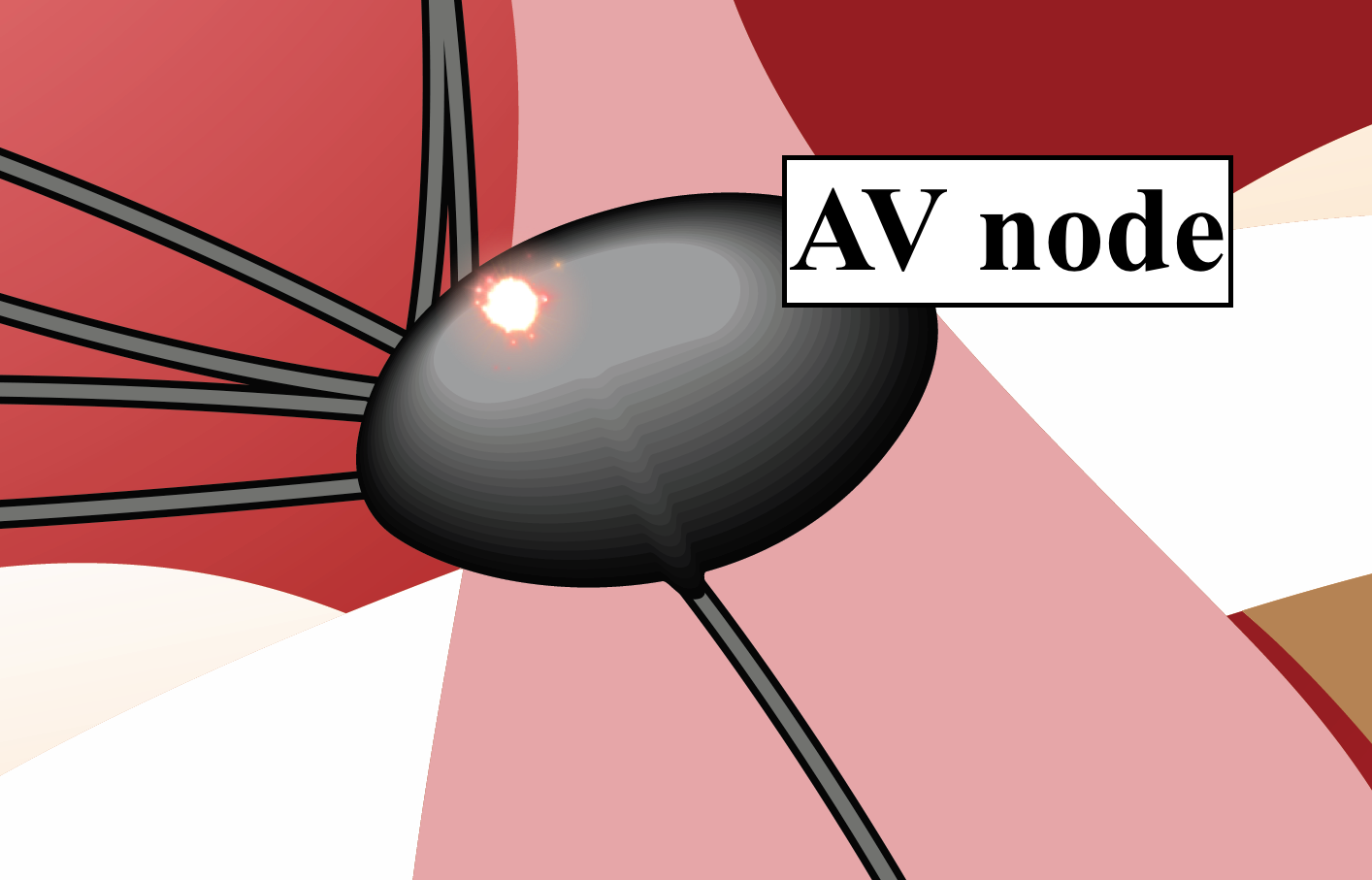
In this situation, the location within the AV node where the "pacemaker" is situated is near the
top of the AV node. Therefore, the electrical signal will escape out the top of the AV node first, and will travel down (slowly) through the AV node and escape out the bottom of the AV node second. The signal that escapes out the top of the AV node will produce a P wave. The signal that escapes out the bottom of the AV node will produce the QRS.
The normal "delay" through the AV node that we see when a signal travels from the SA node down through the AV node is lost in this situation. The P wave and the QRS will occur very close in time to each other.
Therefore the PR interval will be short. Further, the P wave will travel "up" through the atria (in contrast to travelling "down" the atria as when the SA node is the pacemaker). Therefore, the P wave will be travelling in the opposite direction compared to normal and this typically creates an
inverted P wave.
P wave simultaneous with the QRS:
In this situation, the location within the AV node where the "pacemaker" is situated is near the
middle of the AV node. As a result, the electrical signal will escape out the top and bottom of the AV node at the same time. This means that the P wave and QRS will occur at the same time. The QRS is much larger than the P wave and as a result, the P wave is completely obliterated and therefore
the P wave is not seen.
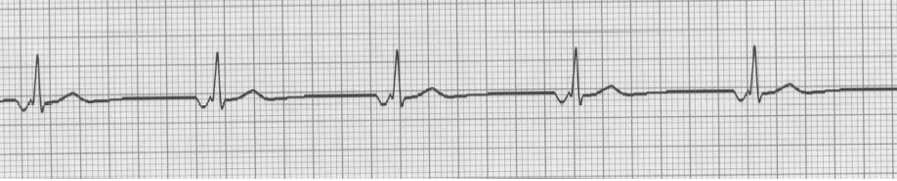
 P wave after the QRS:
P wave after the QRS:
In this situation, the location within the AV node where the "pacemaker" is situated is near the
bottom of the AV node.Therefore, the signal will escape out the bottom of the AV node first, generating the QRS. A very short period of time later, the signal will escape out the top of the AV node and
create a P wave that is AFTER the QRS. In this situation,
the P wave is seen in the ST segment and
is typically inverted.
The red circle highlights the P wave.
 Clinical Significance:
Clinical Significance:The AV node can function as the pacemaker if the SA node is not firing fast enough. The AV node will not be the pacemaker if the SA node is pacing faster than the instrinsic rate of the AV node. The fastest pacemaker "wins", and resets the other pacemakers.
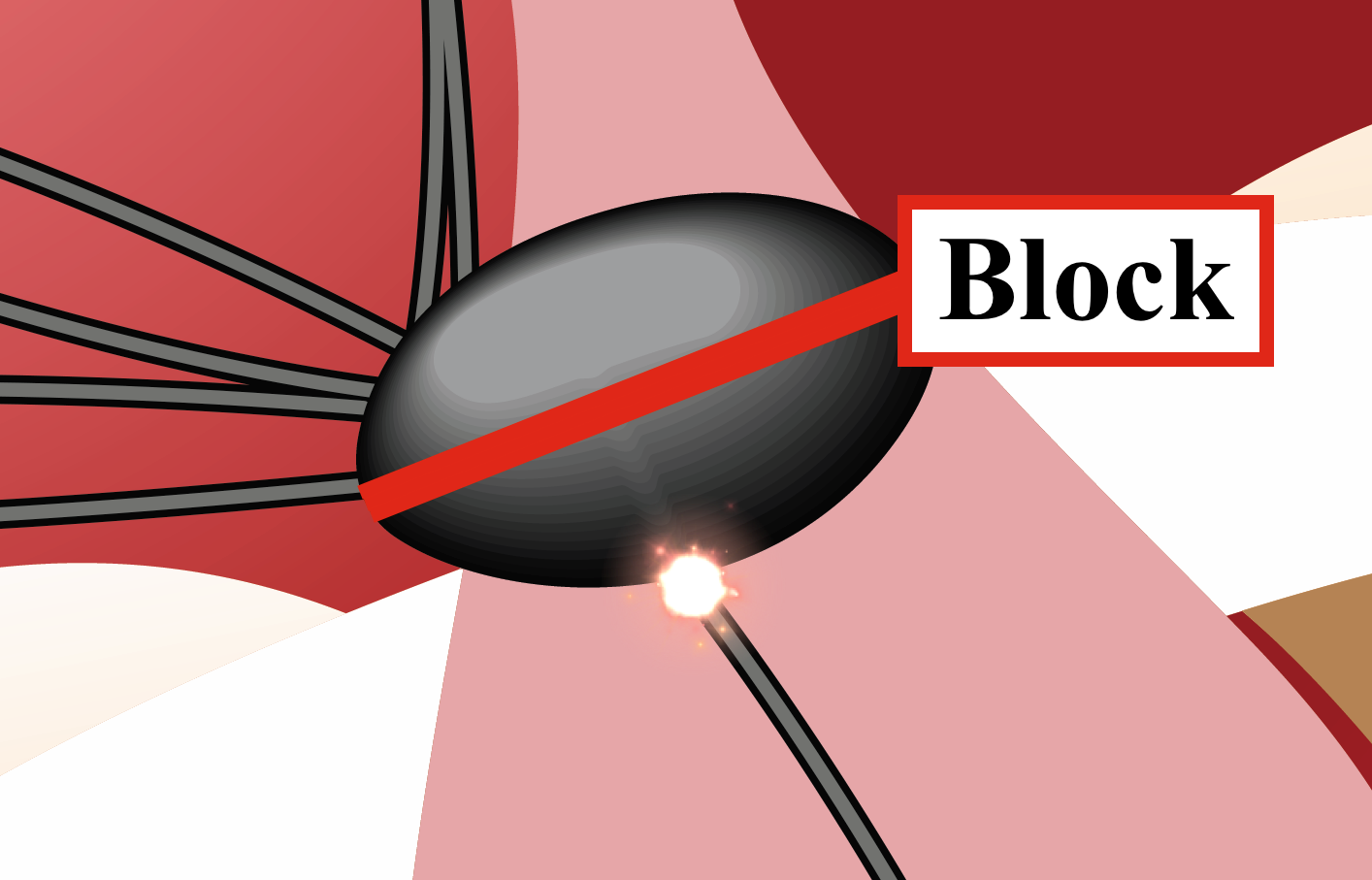
A junctional rhythm can also occur when there is heart block (also called 3rd degree heart block, AV dissociation, or complete heart block). In this situation, no electrical signal passes through the AV node. If the lower portion of the AV node or the Bundle Of His generates an action potential, then the pacemaker that creates the QRS will be the AV node and this would be called "third degree heart block with junctional escape".
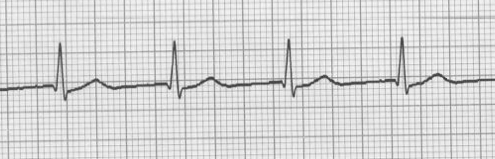
Short PR interval, rate is faster than "normal" AV node, so this is "accelerated junctional" rhythm.
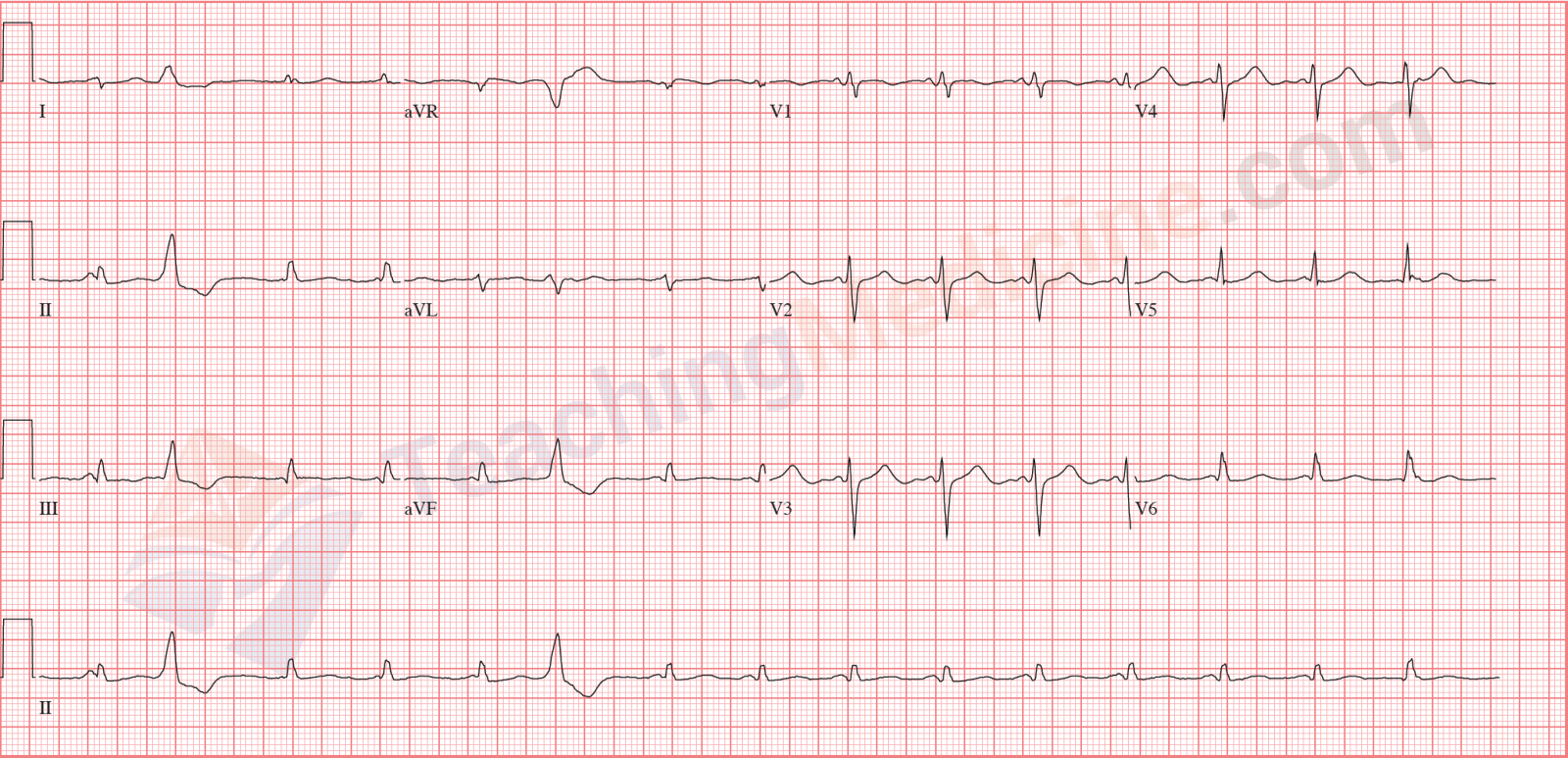
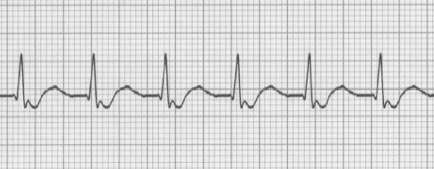
No P waves.
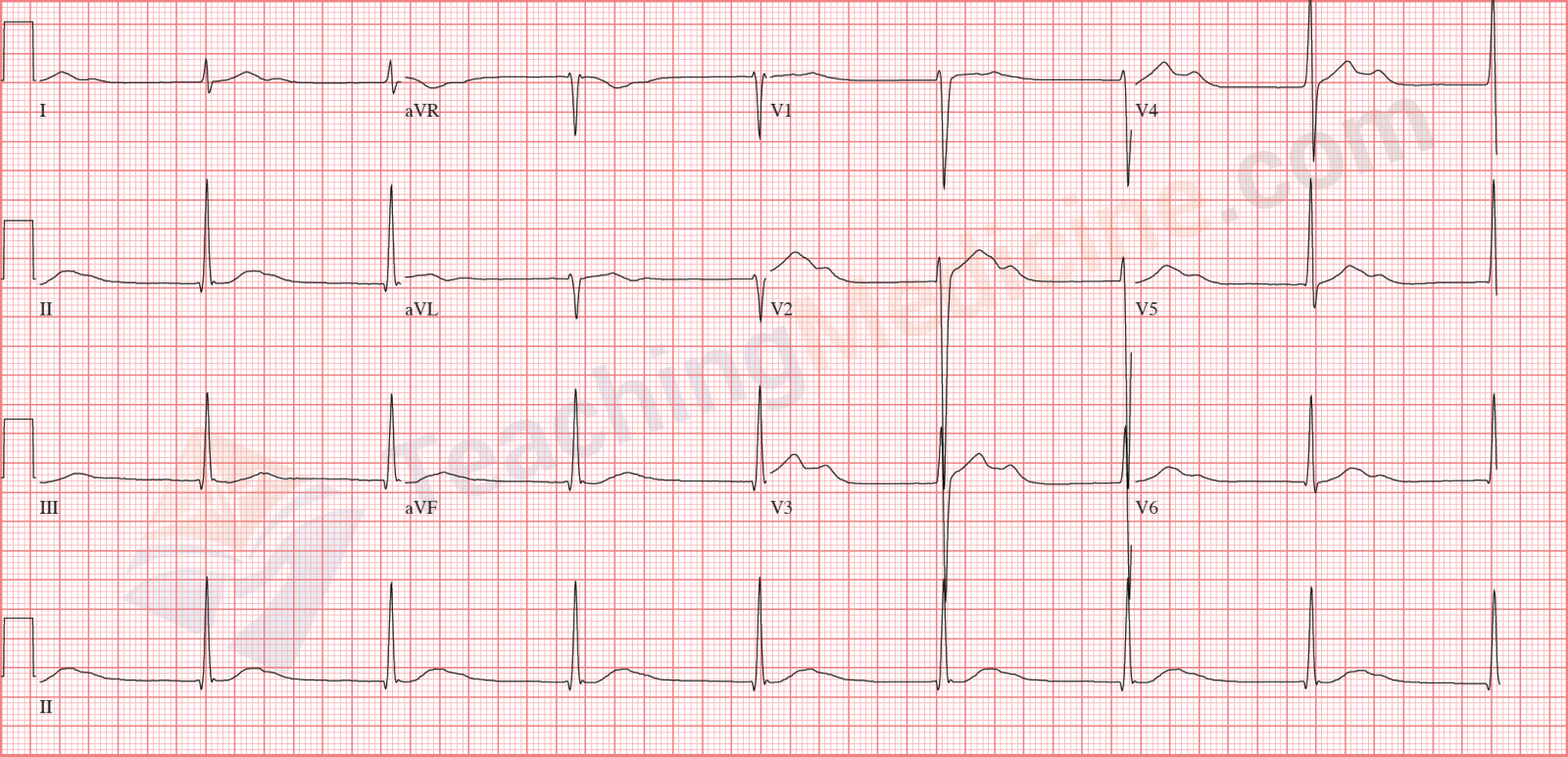
P waves are AFTER the QRS, superimposed in the ST segment (a little bit hard to see).
PR interval is "not applicable".
Rate is faster than "normal" AV node, so this is another "accelerated junctional" rhythm.
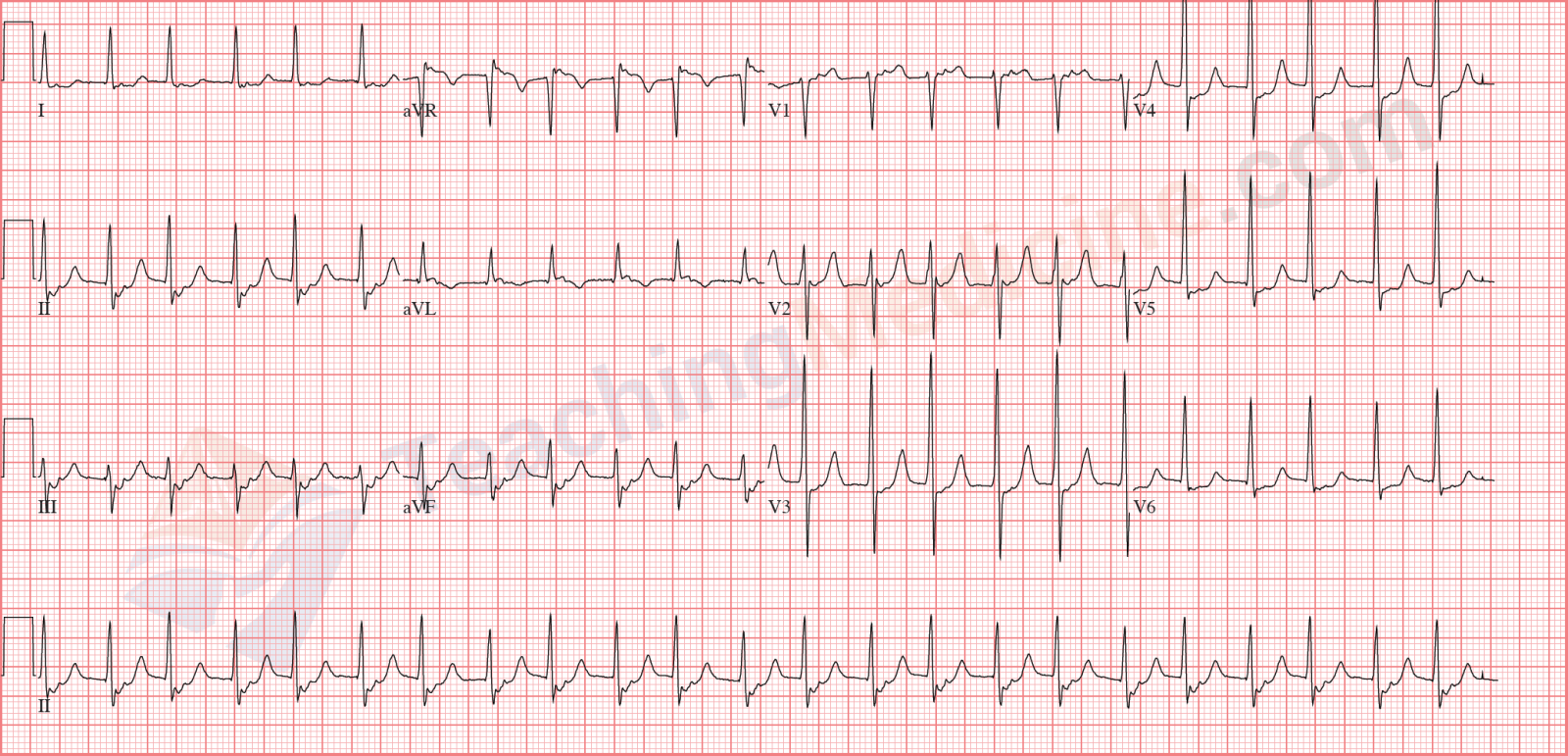
P waves are not associated at all with the QRS, so PR interval is "not applicable".
This is third degree heart block, with a junctional escape.
Often, third degree heart block will have a junctional (narrow QRS) or ventricular (wide QRS) escape rhythm.