Third degree Heart Block Diagnostic criteria: (boldfaced with * indicates an important feature)- * Rate: ventricular rate is almost always slow
- * Rhythm: usually regular but sometimes irregular
- * P waves: more P waves than QRS, P waves not associated with QRS complexes
- * PR interval: not applicable because the P waves are not associated with QRS complexes
- QRS: narrow or wide
ElectrophysiologyIn third degree heart block, none of the P waves are conducted down to the ventricles. In contrast, in first degree heart block, all the P waves are conducted
and in second degree block, some but not all the P waves are conducted.
There are a few names for this heart block. They include:- complete heart block
- A-V dissociation
- third degree heart block
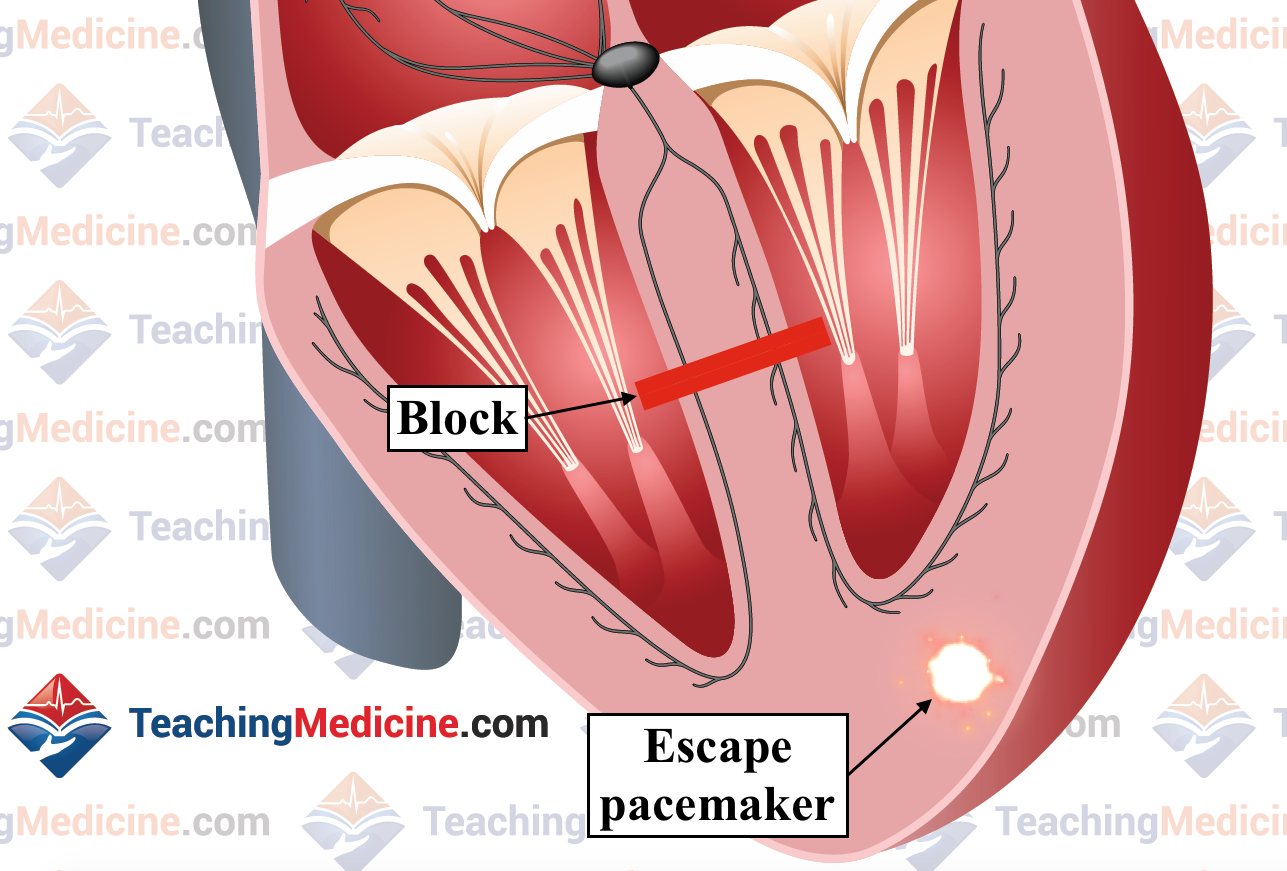
So if none of the P waves are conducted to the ventricles, then which electrical signal creates the QRS complexes? The answer is that there must be 2 different pacemakers that are active during 3rd degree heart block. One pacemaker (almost always the sinus node) gives rise to the P waves. However, these impulses are not conducted to the ventricles because the signal stops at or below the AV node, so a second pacemaker that is BELOW the level of the block must become active and generate the QRS complexes.
This "escape" pacemaker could be in the Bundle of His or it could be in the ventricle. If the level of the block is in the AV node (middle image) or the Bundle of His (3rd image below), then the escape pacemaker is usually in the Bundle of His. In this situation, the ventricular depolarization will occur via the fast conduction fibers and the QRS will be narrow.
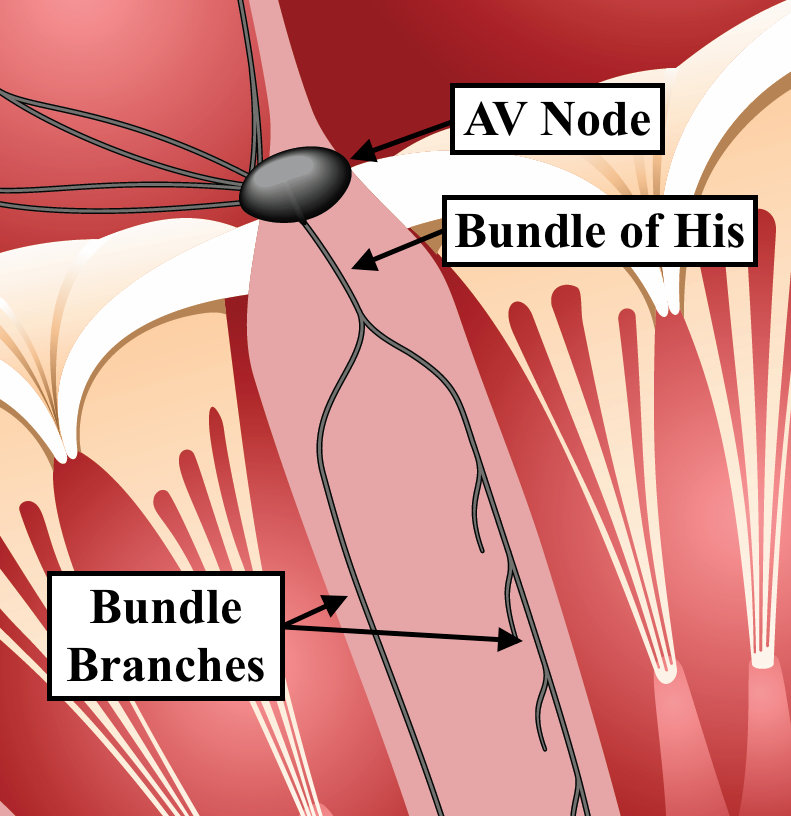
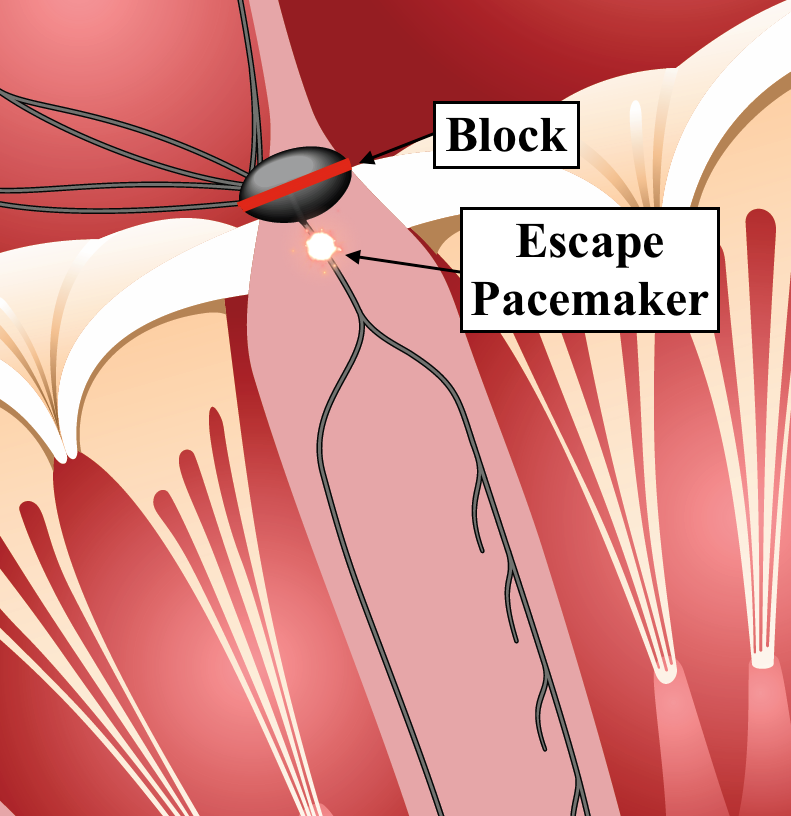
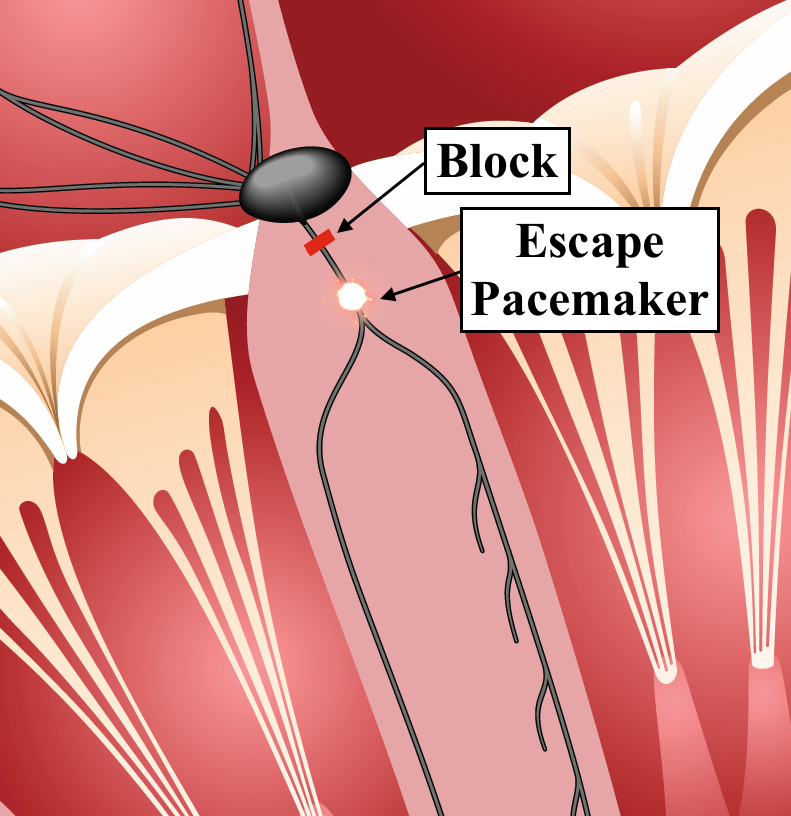
If the level of the block is at the level of the bundle branches (image below), then the escape pacemaker is usually in the ventricle and the QRS complexes will be wide.
In all cases, we would expect the
ventricular rate to be much lower than the
atrial rate because the atrial rate will be created by the SA node which is faster. For this reason, there are more P waves than QRS complexes.
Sometimes, people get tricked when they look at 3rd degree heart block. The reason is that there are usually 2 regular rhythms: the P waves and the QRS complexes, each beating at a different rate. Over time, it is inevitable that
a P wave will occur right before a QRS and will appear as if that P wave is conducted down to the ventricles. Do not be tricked by this. The way to help you avoid this trap is to recognize that
there is no consistent PR interval. You might see 1 or 2 "appropriate" PR intervals, but the fact that they are not consistent should strongly suggest to you that the association of those P waves and the QRS complexes
does not indicate that there was conduction from the P wave to the QRS.
The absence of a consistent PR interval is an important clue that should make you think about third degree heart block. The PR interval is worth a lot of money!If there is no escape pacemaker causing QRS complexes, then the ventricular rate will be zero and the patient will be in cardiac arrest, with no heartbeats. This condition is called
ventricular standstill. It is an emergency because there is no circulation and the brain will likely be damaged within 4-5 minutes of no circulation. This condition requires a "code blue" be called, CPR, resuscitation medications, and electronic pacing (using transcutaneous or transvenous pacing).
Clinical Significance:Third degree heart block almost always causes severe bradycardia that is symptomatic. Patients will have a very low heart rate and as a result, have very low cardiac output and low blood pressure. They will often feel weak, dizzy, intolerant to physical activity, short of breath, and can have angina due to reduced blood flow through the coronary arteries.
Causes of Third degree heart block:- ischemia or infarction (the AV node branch of the right coronary artery usually supplies the AV node)
- fibrosis or sclerosis of the conducting fibers (many causes)
- heart surgery
- cardiomyopathy (a generic term to describe disease of heart muscle ... many causes of this as well)
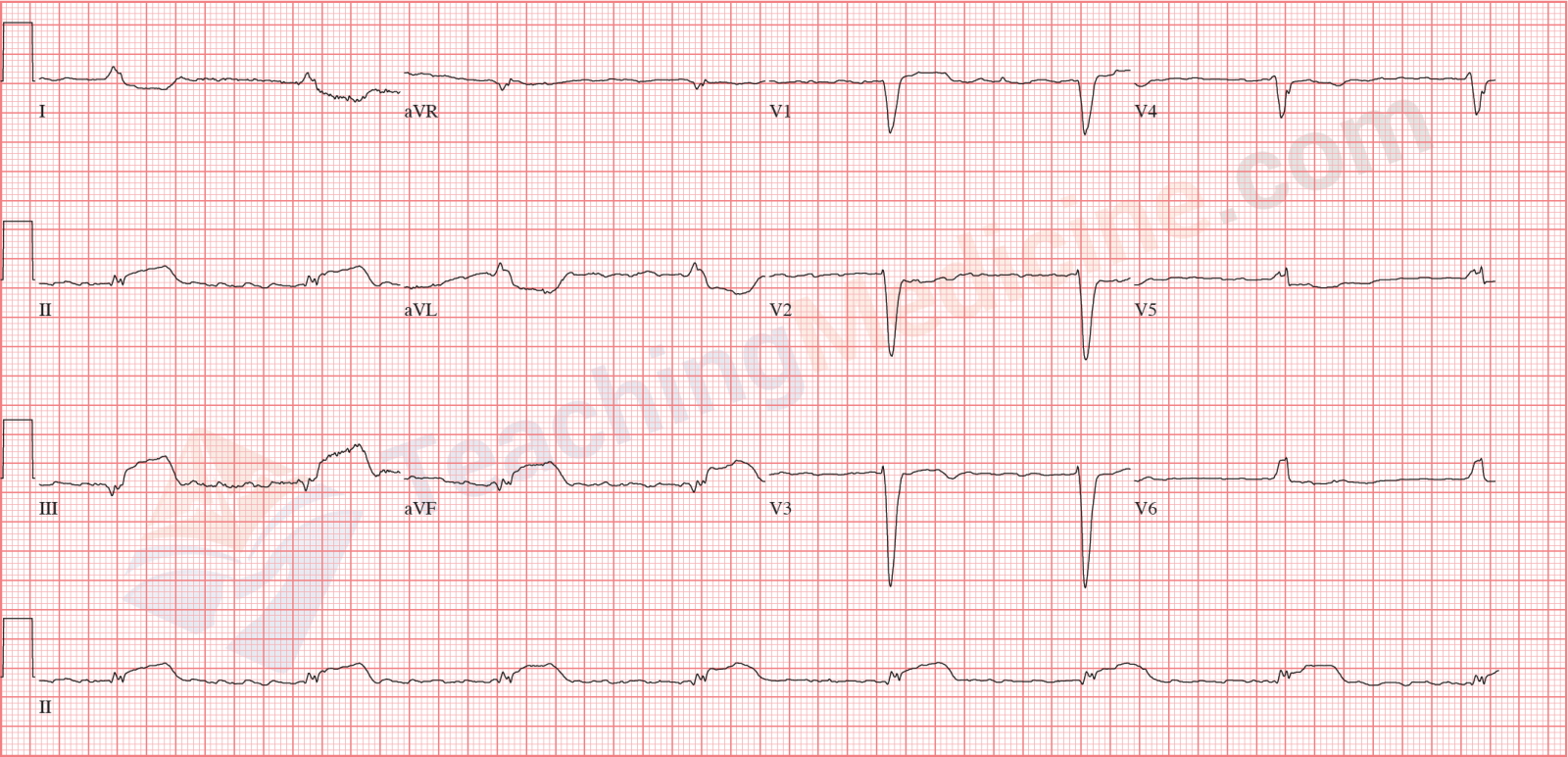
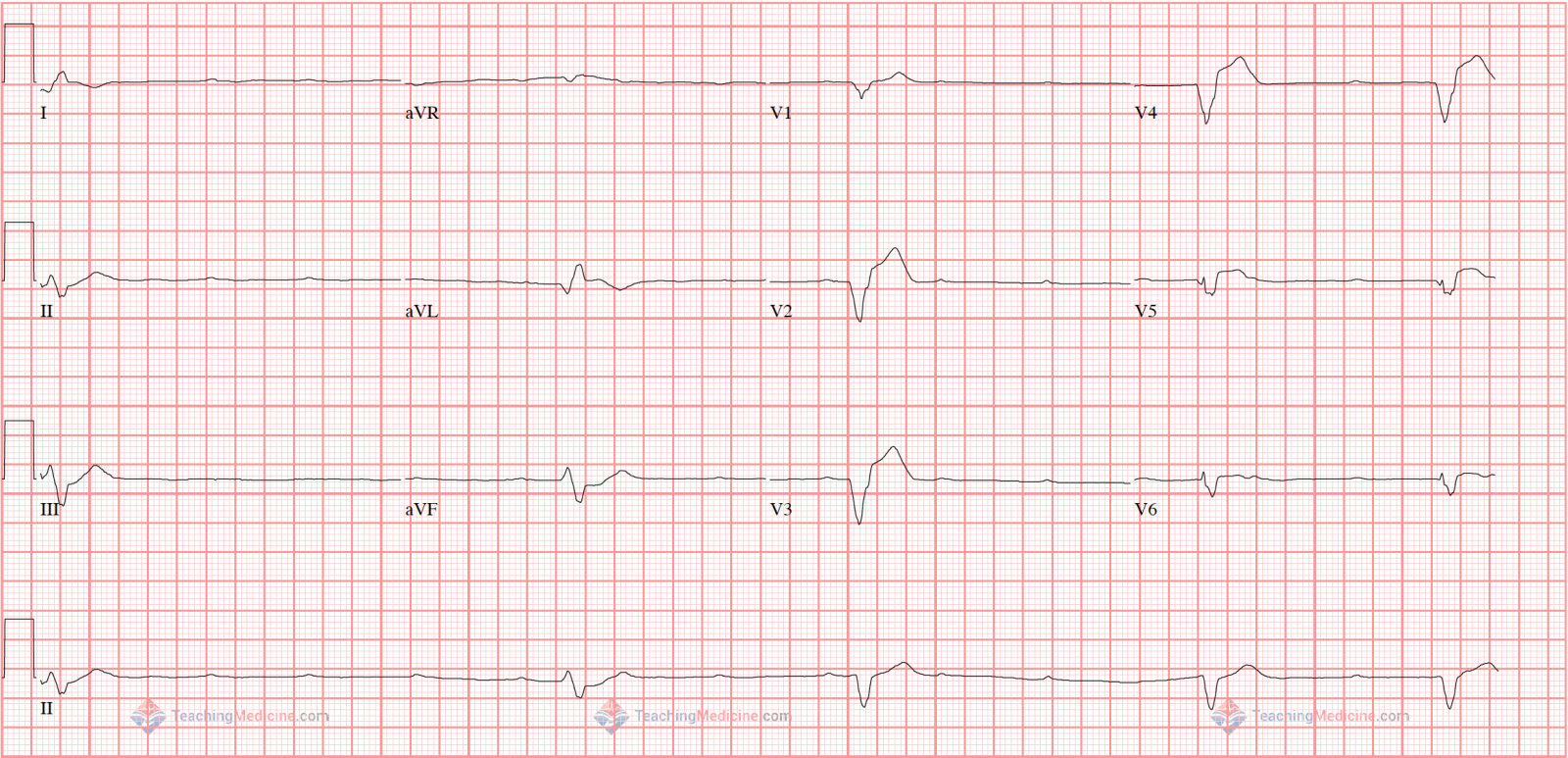
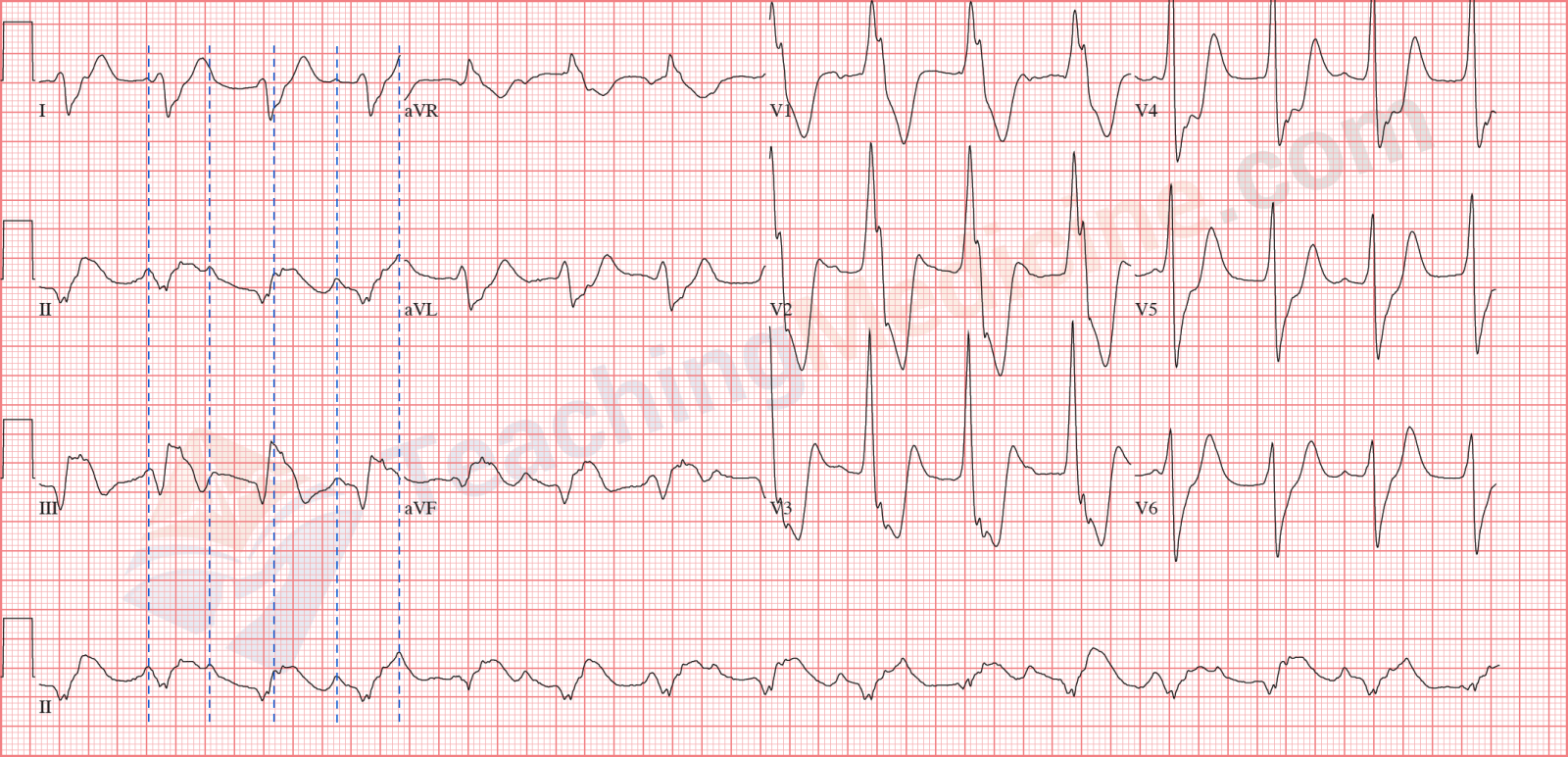
Examples:Note that the QRS is wide and the ventricular rhythm is not regular. P waves easily seen and clearly not conducting down to the ventricles.
QRS is narrow and again, not completely regular. The key is that there is no association between P waves and QRS.
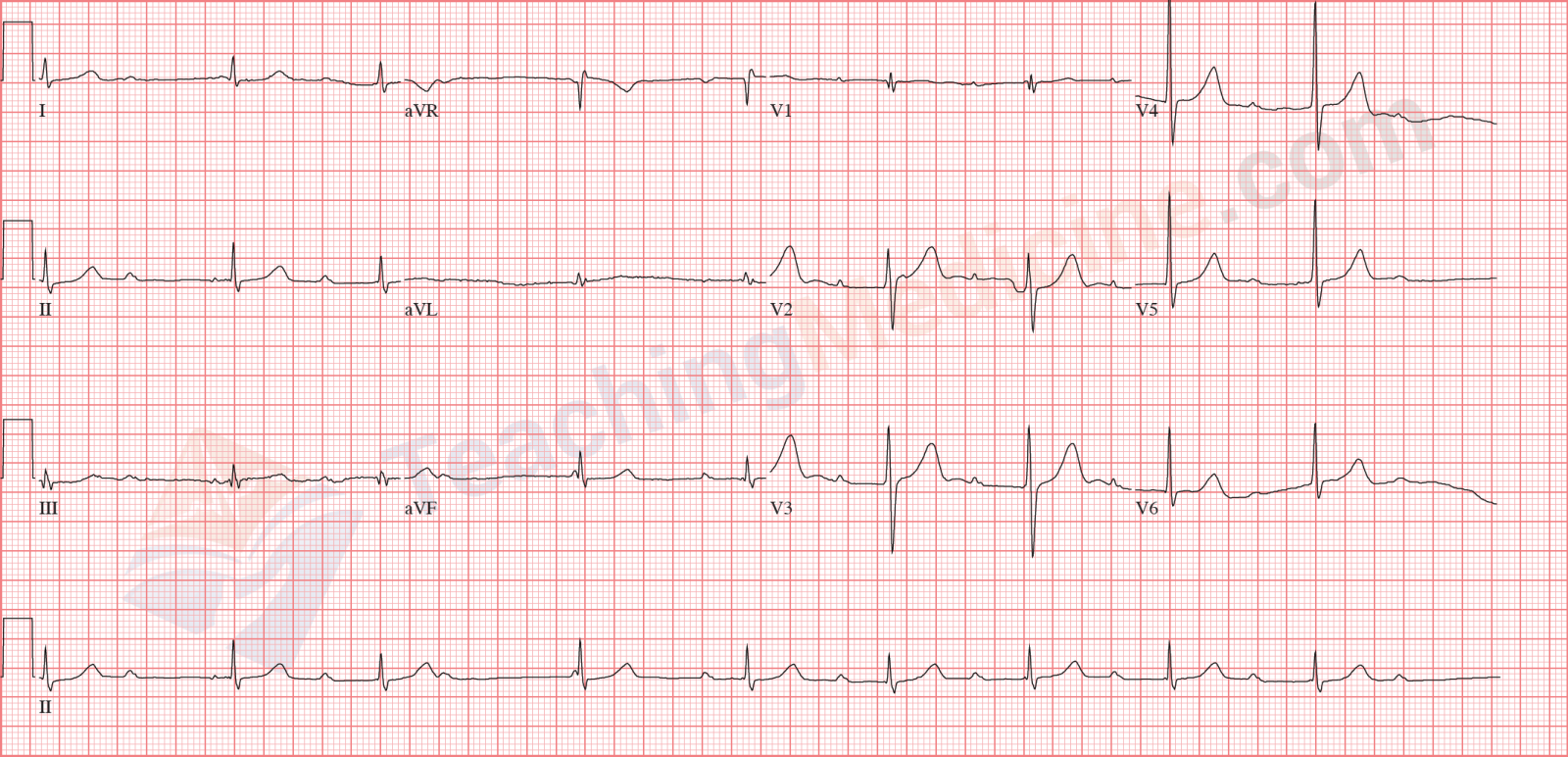
Don't let your eyes be distracted by the ST segment abnormalities (which are severe). Narrow QRS and no association between P waves and QRS.
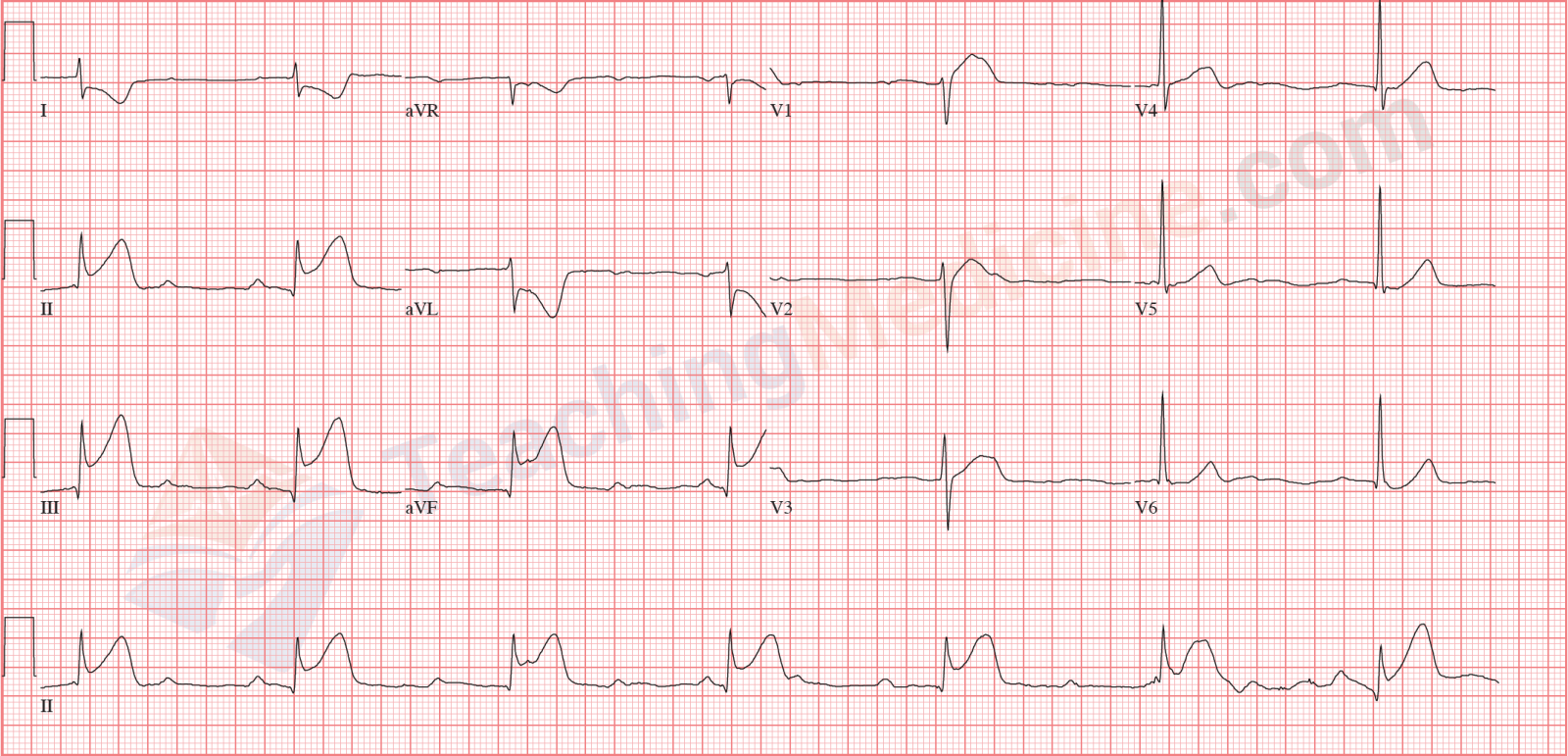
Having trouble seeing the P waves here? I drew 4 vertical blue lines to indicate the first 4 P waves. Can you see the others?
None of them are associated with the wide QRS.
Ok. This one is really tricky. There are no P waves. Do you see the wavy baseline? This is atrial fibrillation with third degree heart block. Remember that atrial fibrillation should have a ventricular rhythm that is irregular with no pattern. This ECG is very regular. If you thought this looked like a junctional rhythm with artifact, you can't be faulted for thinking this. Experience is needed to help tell the difference between the artifact and fibrillation.