Lesson 5: Collaborative Decision Making & Mutual Support 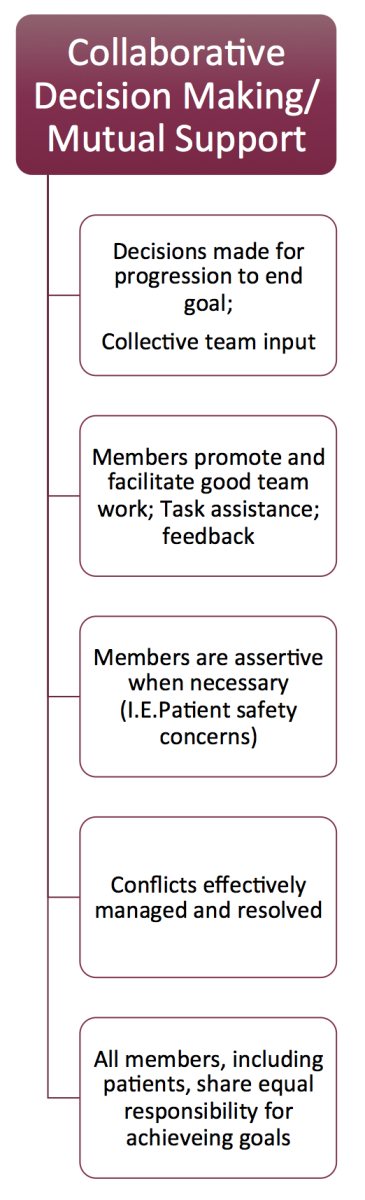 At the end of this module, you will:
At the end of this module, you will:- Understand the elements of Collaborative Decision Making/Mutual Support
- Consider specific teamwork strategies to improve Collaborative Decision Making and Mutual Support
- Consider examples of how you might apply effective collaborative decision making and mutual support skills to clinical practice
Decisions are made for progression to the end goal with Collective Team Input:It is important that a leader states the goal and frequently updates the team.
A leader needs to
invite and respect the opinions of team members to encourage a team that is psychologically safe to work collectively.
This requires a
culture in which collaborative decision-making is stated as the norm, and is taught and reinforced at an organizational level.
Key Point:The patient and family represent key members of the health care team and seeking their input is of equal importance. Time for Reflection: How do you ensure the patient and family are integral members of your health care team? How do they help guide the teams’ decision making process in a collaborative and integrated way?
Members Promote and Facilitate Good Team work (Task assistance & Feedback)Interprofessional collaboration requires team members to learn about, from and with each other (12) . Trust and psychological safety are needed in order to feel safe to offer and accept feedback, or ask for assistance from other team members.
Creating a “culture of teamwork” requires practicing together and honoring teamwork in your institution. This is especially valuable with healthcare teams that are formed rapidly in most cases (not always the same team members). The more that you practice task assistance and feedback (and accept it), the more you contribute to this culture.
For Example:By developing simulation and debriefing programs at your institution, team members can come together to practice, make mistakes and learn from them in a non-judgmental environment. This culture of safety will ideally carry over to the bedside.
Members are assertive when necessary to advocate for patient safety We know that there is hierarchy in healthcare and that it is commonly reported that health professionals are challenged with speaking up. Challenging a leader, especially if a senior, can be very intimidating. When
specific rules and language are promoted and practiced, the focus can remain on patient safety rather than on individual performance or personalities.
One standardized “
Critical language” tool is called ‘
CUS”. It is outlined below and can be helpful when a member of the team feels unsafe about a situation and wants to get the leader and/or team’s attention. Although it might feel that you are being ignored, there are many reasons why a person might not be heard in a critical situation including competing stimuli, fatigue of team members, or fixation error. The critical language allows for a succinct and clear escalation of a concern. The team member initially states his/her concern and if there is no acknowledgement and action, then the concern needs to be escalated to state “I am uncomfortable”. Finally pointing out that there is a safety issue is often enough to get the attention of the team. (4)
- C: “I am concerned…
- U: “I am uncomfortable…
- S: “This is a safety issue
Common Pitfall:Critical Language tools are the most effective if the entire team acknowledges this as a form of communication during difficult times. Your organization needs to build a culture of safety around these principles.
Conflicts are Managed and Resolved Interprofessional Conflict Resolution may be one of the most difficult things to manage and a common challenge for many teams.
Conflicts can be proactively managed with the above teamwork skills including role clarity, clear communication and a collective orientation.
However, conflict in teams will still occur and specific strategies can be learned to help negotiate difficulties with colleagues. Success in this area promotes the culture of safety and teamwork. Unresolved conflicts will erode the culture
Time for Reflection: How do you identify and approach Interprofessional Conflict?
Do you value the potentially positive nature of conflict?
How does conflict impact team function?
All members, including patients, share equal responsibility for achieving goals. Highly effective teams are described as those that have a
collective orientation. Everyone shares responsibility for success.
ONE of the five key impediments to effective communication in the clinical setting (13) is the fact that team members are educated in their respective disciplines in a siloed manner, with the result being ingrained assumptions about the other.
Key Point:The highest functioning teams need to PRACTICE their teamwork skills together! As suggested by the Institute of Medicine, the use of Simulation focused on improving teamwork is one mechanism to improve patient safety. Simulation allows us to learn about, with, and from each other and practice our teamwork skills such as leadership, roles, communication, situation awareness, and resource utilization on Interprofessional teams.
Acknowledgements:Kristin and Mirette would like to thank the following people for their contributions:
Dr. Jason Waechter; Dr. Nishan Sharma; Dr. James Huffman; Dr. Jason Lord; Dr. Ian Rigby; Dr. Start Rose; Cherie Serieska; Sue Barnes; Ken Brisbin; Dan Huffman; Tanya Platt;
Marlene Donahue; Dr. Adam Cheng; Marlene Donahue; Dr. Alyshah Kaba
Mirette and Kris would like to thank all authors and reviewers of the multiple choice questions including Sue Barnes, Dr. Adam Cheng, and Dr. Alyshah Kaba. “We must all hang together or most assuredly we shall all hang separately.” -Ben Franklin