Lesson 3: Situation Monitoring 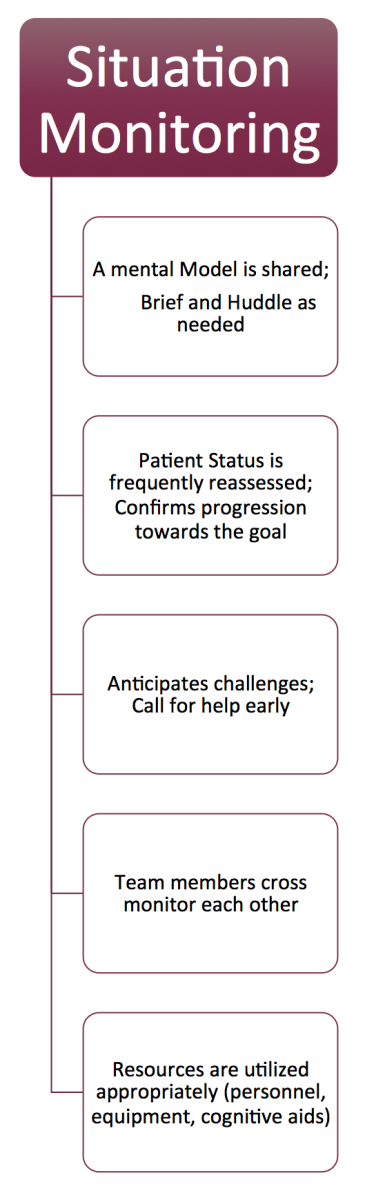 At the end of this module, you will:
At the end of this module, you will:- Understand the elements of Situation Monitoring
- Consider specific teamwork strategies to improve team situation monitoring
- Consider examples of how you might apply effective situation monitoring skills to clinical practice
Situation Monitoring is defined as maintaining the “big picture” perspective that is best supported by actively reassessing/reevaluating the circumstances.
Essentially, a team needs one person to take responsibility for:
- Knowing what is happening from the patient and overall team perspective
- Understanding what it means and,
- Anticipating next steps and potential problems.
A Mental Model is Shared; Brief and Huddle as Needed:A Mental Model: is a psychological representation of the current situation as understood by the leader. In simpler terms, what the leader thinks is going on with the patient.
Briefing is what you do before going into a situation so you are all “on the same page” or have a shared mental model about goals, potential risks and contingency plans (7).
A
huddle, sometimes called a
summary, can happen at any time throughout the team’s process of caring for a patient. Its purpose to keep everyone “on same page” by establishing a shared mental model. It can be particularly helpful to huddle when a patient condition changes or after several simultaneous tasks are completed.
For Example:The team leader refocuses the team by saying something like:
- Here’s what I think we face . . .any other ideas?
- Let’s take a minute to get on the same page here. . .
- Let’s recap…
Ideally, leaders will communicate the next 2-3 priorities at the end of the huddle for the team.
A verbal summary or huddle can get everyone up to date and moving toward a common goal. If a leader is having difficulty, asking for team input and talking out loud can help the team to strategize solutions together.
Similarly, if a team member is unclear on the overall plan, then they can request a “huddle” when time permits.
Patient Status is Frequently Reassessed; Confirm Progression Towards the GoalFrequent reassessment of the patient (and not just the team members!) is important to ensure that progress is being made. The team goal should also be clear.
Reassessing is essential after key interventions or after a change in patient condition. Reassessing the patient often refocuses the team in the same way that a “huddle” will.
Anticipate Challenges; Call for Help EarlyMany highly functioning healthcare teams have created a deliberate “pause” or “time-out” to ensure that challenges are anticipated (for example, before intubation or before surgery is commenced). During such a “pause” the plan is described, challenges are identified and a back up/ contingency plan is identified. This helps the team to anticipate difficulties early so as to be prepared. (8)
Key Point: “Calling for help is not a sign of low self confidence; it shows your sense of responsibility and respect for your patient’s safety. Heroes are dangerous! (9)
Team Members Cross Monitor Each OtherAny team member can become fatigued, task- focused or fixated.
Fixation error occurs when a practitioner fails to revisit the big picture even when there is data suggesting that the current mental model might be incorrect. For example, it is essential to keep a broad differential diagnosis even after the initial assessment strongly suggests a particular diagnosis and course of treatment. When a team member becomes overwhelmed or fatigued they can take much longer to complete a task, can lose sight of the overall goals of the team, and can stop communicating effectively with the rest of the team.
Team
cross- monitoring is the best way to ensure that we recognize and correct these potential pitfalls in our teammates. If a team member is not performing optimally for any reason, it is essential that team members support them for the ultimate success of the team’s performance.
Support can come in many forms including
physical (take over CPR compressions of a colleague who is tiring),
cognitive (suggest that it might be time for a full reassessment given that the patient is not responding as expected to the intervention) or
collaborative (point out to the RN responsible for meds that you are not busy and available to help with the multiple orders she has received).
Resources are Utilized Appropriately (Personnel, Equipment, Cognitive Aids)Knowing what resources are available to you and how to access them is essential. This includes people both in the room and available to help if needed, equipment and where it is located, and the use of cognitive aids for diagnosis and/or management.
Common Pitfall:Using a cognitive aid for the first time during a high stress emergency situation is
not a good idea. The additional mental work of engaging with unfamiliar material is very likely to overwhelm the team member rather than help with problem solving. It is essential to know how to access important cognitive aids in your area of work, and to
practice using them before you rely on them in clinical practice.
Key Point:Looking something up, or following a cognitive aid can save a life. Don’t try to impress others by attempting to remember everything! Be safe!