Lesson 2: Communication
 At the end of this module, you will:
At the end of this module, you will:- Understand important elements of communication for a well-functioning, competent team
- Consider specific teamwork strategies to improve team communication
- Be able to provide examples of how you might apply effective communication skills
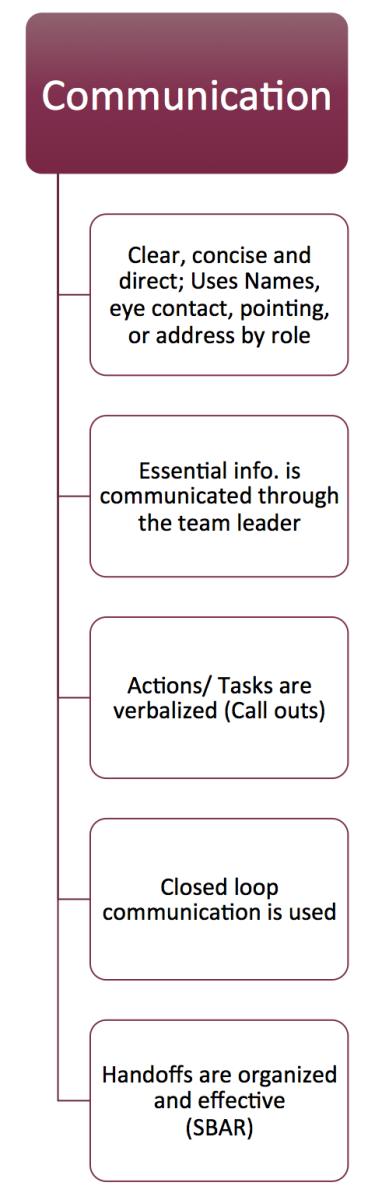
Clear, Concise Communication:Even though it may feel awkward, effective communication may need to be very
direct.
What does Direct Communication look like?
- Use names or call out by professional roles to identify people.
- Make eye contact and point if necessary, or describe what people are wearing.
- Speak clearly and concisely!
Common Pitfall:Avoid requesting: “can SOMEONE get me the….”
For example: In a cardiac arrest resuscitation, the leader asks for
“someone” to call for help. Now one of two things can happen: either no one receives the message and no one calls for help; or several people unnecessarily leave the room to call for help thereby reducing the number of available resources in that moment.
Essential Information is communicated through the Team Leader:A collaborative leader supports shared decision-making by deciding on the best course of action after considering input from the team. This means that all team members are accountable for speaking up, for contributing to decision making and for fulfilling their roles and responsibility within their scope of practice.
Once a team is made up of 2 or more, there needs to be a single “leader” who ensures that the
essential information is incorporated into decision making. Side-bar communication between caregivers might be required for the completion of some tasks, but ultimately one person needs to maintain a global perspective, or situational awareness.
For Example: In a resuscitation, two nurses will often work together to ensure that the calculation of an ordered medication dose is correct, but the leader needs to be informed directly once the drug is prepared and ready for administration.
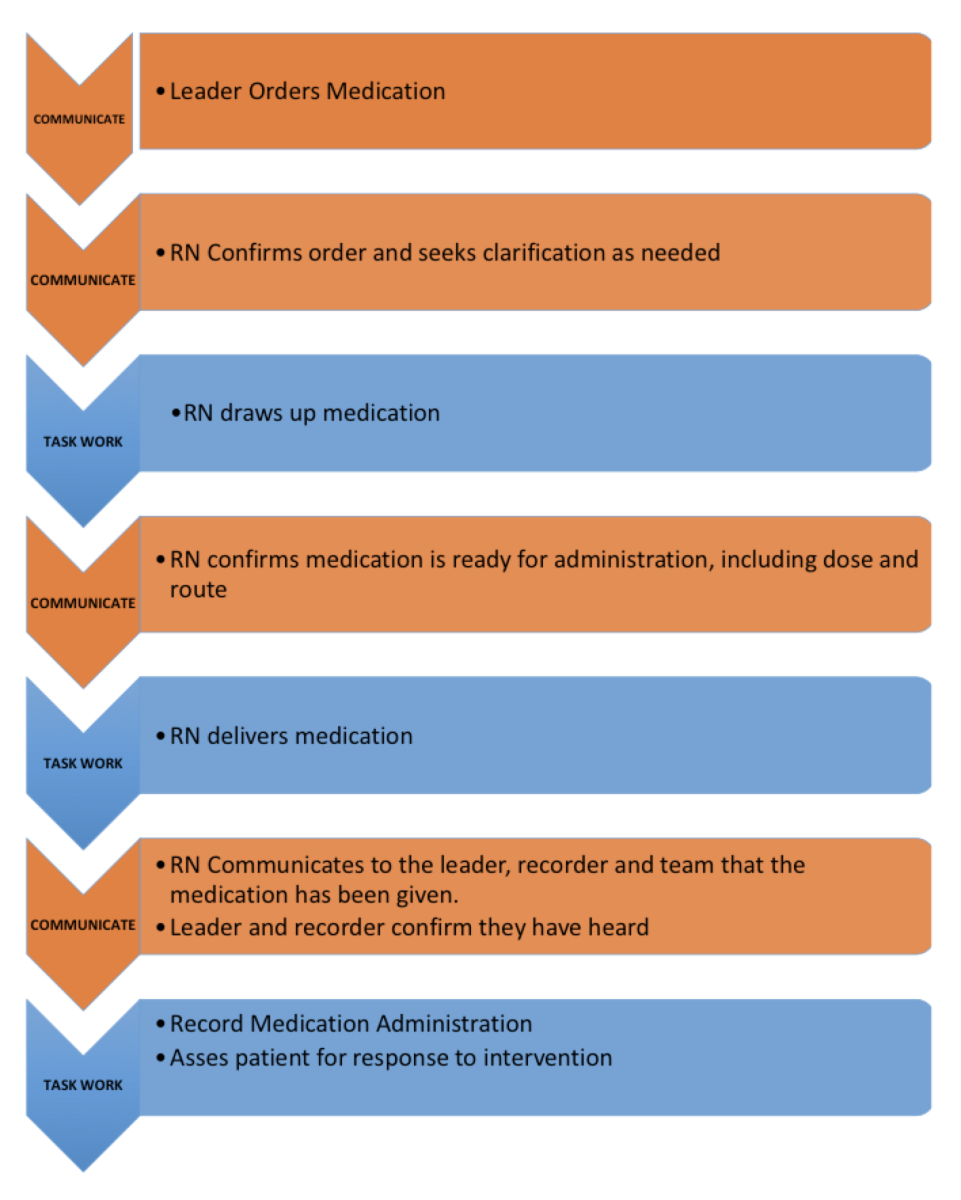
Actions/Tasks are verbalized (Call outs): Leaders are required to process large amounts of information when overseeing an interprofessional team. Even if the leader is looking right at you, they might not always notice exactly what you are doing or even saying to them. For this reason, communication during team activities must be explicit and confirmed. Using closed loop communication is very effective in ensuring tasks are completed and that all team members know the current status of the team. The figure below outlines one example incorporating essential elements of
closed loop communication. (6) Notice that for each task completed (blue) there are one or more essential communications(orange) that need to occur.
 Common pitfall:
Common pitfall:Failing to "close the loop" at each of these stages of patient care is a common and dangerous error.
“Forgetting to Close the Loop” Example: A physician orders a medication for a patient in cardiac arrest. The RN acknowledges the request but needs to leave the room to obtain the medication. Upon return, she does not realize that the patient has deteriorated and no longer requires that specific therapy. She spends time mixing and hanging the medication before reporting that the task is completed, at which time she is told that in fact, that medication was no longer needed. At best, the team has wasted valuable time, at worst there could be an adverse effect of the unnecessary medication.
Time for Reflection: How do you ensure that the message you intended to deliver was the message that was understood by the individual who received it?
Handoffs are Organized and Effective:“Handoff” or “Handover” occurs when the responsibility for patient care is transferred from one caregiver to another; this happens thousands of times every day in our hospitals. This is what we know about handover (7):
- It is a major source of potential error for many reasons including time limitations, cognitive limitations, and human error.
- There are more handovers now than in the past because of work hour restrictions and increasing complexity of patient care. Fortunately, there is a growing body of literature about the common pitfalls and potential tools to mitigate risk to patient wellness.
- Using a standard form of communication creates a shared expectation between sender AND receiver of information. Handover tools promote critical thinking, reduce cognitive workload for users and encourage a common lexicon for healthcare teams.
The SBAR tool(4) is one commonly used approach to standardizing and improving handover between caregivers. It is a commonly used tool that should only take 60-90 seconds to relay information to another caregiver in an organized way. Here is the structure of SBAR:
S - Situation: State the facts about what is happening at the present time that is of importance to communicate. What is your major concern?
B - Background: Explain circumstances leading up to the situation. Put the situation into context for the reader/listener. What are the most important facts?
A - Assessment: What is the current problem or important potential problem in the near future?
R - Recommendation: Explain your plan for the patient. How can the team mitigate any existing risks?
For example, with our patient in heart failure, an SBAR of an RN updating a team member who is entering the room 30 minutes into the resuscitation might sound like:
S - Situation: This is Mr. Smith. He is a 75-year-old gentleman with recurrent heart failure. His code status is “full code”. He received his diuretic 30 minutes ago but we are concerned because he is not responding and he is quite hypoxic.
B - Background: He is a known cardiomyopathy with 6 prior admissions this year. He has renal failure and we are waiting on his blood work. He did require non-invasive ventilation during his last admission.
A - Assessment: Dr. Jones thinks that the diagnosis is heart failure but is concerned that he is not yet responding to therapy. We’ve just given him another dose of Lasix and some Nitroglycerin. His vitals are: HR 110; BP 90/60; RR 28; SpO2: 88% on 60% Oxygen. He is afebrile and drowsy but rousable. We need to continuously monitor his vital signs for hypotension and hypoxemia.
R - Recommendation: We are pretty sure he is going to need non-invasive ventilation. I’ve called the Respiratory Therapist and they are coming to assess and perform arterial blood gas analysis. In the meantime can you please insert a foley catheter to help with monitoring the effect of the diuretic?
Key Point: The several handovers that occur during a patient journey, increase the risk for miscommunication and loss of vital patient information.Ideally, you should plan your
approach to communicating critical information as well as the content of the handover before you relay it to another healthcare team member. SBAR can help!